Would you accept a transfusion of blood products from a chimpanzee or a gorilla? Or what about a pig? One person did back in 1667 when French physician Jean-Baptiste Denis successfully transfused blood from a lamb into 15 year-old human boy. This may surprise many people as most are aware that even humans are not universally transfusion-compatible. Instead, humans are divided into blood groups that determine who can receive blood from whom without suffering a severe immune reaction that can be fatal. That’s because our immune system senses molecules on the surface of red blood cells and reacts aggressively to certain surface molecules, or markers, in an individual whose on red blood cells don’t have the same kind.
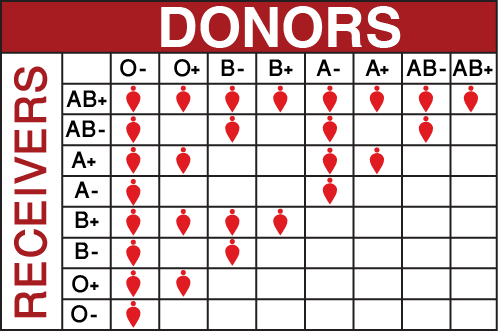 But while there are literally hundreds of different surface markers that make red blood cells different between people, only a handful of markers act as strong antigens to the immune system. The main ones are the ABO and Rh antigens (the positive or negative seen after the more commonly known A, B, O types) and for people to receive blood products they must be appropriately ABO and Rh matched. It turns out, however, that the ABO and Rh blood groups are not limited just to human populations. They also apply to our close relatives in the animal kingdom, especially other primates. Indeed, Rh stands for rhesus, because it was identified on the red blood cells of rhesus monkeys before it was found on human red blood cells.
But while there are literally hundreds of different surface markers that make red blood cells different between people, only a handful of markers act as strong antigens to the immune system. The main ones are the ABO and Rh antigens (the positive or negative seen after the more commonly known A, B, O types) and for people to receive blood products they must be appropriately ABO and Rh matched. It turns out, however, that the ABO and Rh blood groups are not limited just to human populations. They also apply to our close relatives in the animal kingdom, especially other primates. Indeed, Rh stands for rhesus, because it was identified on the red blood cells of rhesus monkeys before it was found on human red blood cells.
All of this means that a human can be ABO and Rh matched for blood products from a monkey, or even better, a great ape such as a gorilla or chimpanzee (who are closer to us on the evolutionary tree than monkeys). And, since the ABO and Rh antigens are the most critical factors to match to avoid fatal transfusion reactions, it means that xenotransplantation from an ape is feasible theoretically. But some hurdles may exist to making it a reality.
Drawbacks to ape blood and benefits of using pigs
Work with blood and non-human primates goes back to Karl Landsteiner, who not only co-discovered the rhesus factor in monkeys in 1937, but also discovered the ABO groups in 1900. The blood group commonality between humans and other animals thus is not a new revelation, but this raises question of why xenotransfusion was not seriously decades ago.
One reason is because, despite ABO and Rh commonality, there are minor differences between the blood of humans, apes, and other animals whose effects on transfusion would have to be understood completely. Humans also may still have some lingering superstitions about blood from non-humans that make xenotransfusion unpalatable. Also, when it comes to great apes, they are endangered. They’re not like cows and pigs that simply are bred in industrial quantities to serve humans. So, even while it might be no more trouble for an ape to donate blood than for a hen to lay eggs, the supply of ape blood would be fairly small anyway.
Thus, as we consider xenotransfusion pigs might actually be a more feasible option, and in fact that’s what’s happening. Xenotransfusion research currently focusses on pigs, not apes, and it’s not just because pigs are abundant. They’re blood actually is quite similar to human blood. The size of red blood cells is similar. So is the typical red blood cell life span, the hemoglobin content and structure, and other factors, plus pigs can be genetically modified to produce red blood cells that are equivalent to human type O negative. As noted earlier, that’s the universal donor blood, and this makes xenotransfusion sound very attractive, although, other ways to make O negative blood also beckon.
Blood product efficiency
Very relevant to the discussion is the question of whether, or to what degree, we even need alternatives to human blood donors. Although there are frequent blood shortages, especially in summer, although the total amount of needed blood has been increasing because the population is growing along with the number of sophisticated surgical procedures (like organ transplants and coronary artery bypass surgery (CABG) that often require many units of packed red blood cells (PRBCs) and other blood products), the amount of blood consumed per capita may actually be starting to decline. That is because efficiency with blood products has increased, due to technological advances for storing blood and getting what we need from it. That fact that we only talk about blood products, such as PRBCs, platelets, or fresh frozen plasma (FFP), rather than whole blood shows how much we’ve advanced since the early 20th century, when transfusion meant taking blood from one individual and infusing it whole and unchanged into a recipient. The system has gained a great deal of specificity.
Blood modification and synthetic blood
Another factor that leads to blood shortages involves blood group compatibility. If you are are type O-negative, that’s the only kind of blood you can receive, but you’re a “universal donor”; people in other groups can receive your blood. If you’re AB positive you can receive blood from nearly anyone in most cases, but your blood can be given only to people of your type. Blood products have a limited storage time before they must be discarded, the proportion of donors versus recipients is not the same for every blood group, and blood groups vary among populations. For these reasons, the very existence of the blood groups reduces efficiency of blood product utilization.
However, biochemically, the difference blood types A, B, AB, and O is not very great. It depends only on a couple of sugars at the ends of chain-like molecules that stick out from the red blood cell surface. Type A antigens have one type of sugar at the end of the chain, Type B antigens have a slightly different sugar at the end of the chain. People with AB blood have both antigens on their cells while those cell of blood type O still have the surface molecules, but without either of those sugars at the end that cause so much trouble in a person who receives the wrong blood. But biomedicine has almost reached a point now where there’s a simple solution. Simply snip off those terminal sugars and any donated blood becomes type O. It works with an enzyme that does the snipping but until recently the process has been incomplete and expensive. The immune system is exquisitely sensitive to ABO antigens, which means if a type A or B blood is converted to give to a type O recipient, the conversion really has to be complete. Every single one of those sugars on every red blood cell must be snipped, or it won’t work. With new biotechnology procedures, it now looks as though the ability to to make full conversion of human A, B, or AB blood to type O is just around the corner, and that might be a lot easier than doing it with blood from pigs. Plus, there is another solution around the corner that could make all of the discussion about alternative donors, whether human, ape, or pig, obsolete: synthetic blood. Just make what we need from scratch, then there are no antigens to worry about, human or otherwise.
All this means is that it’s unlikely you’ll see blood banks and hospitals stocking up on blood products from apes in the near future because many simpler, potentially less macabre options exist. But these non-human animals do constitute a potential alternative source of blood products, if ever the moment comes where they are needed.
David Warmflash is an astrobiologist, physician and science writer. Follow@CosmicEvolution to read what he is saying on Twitter.